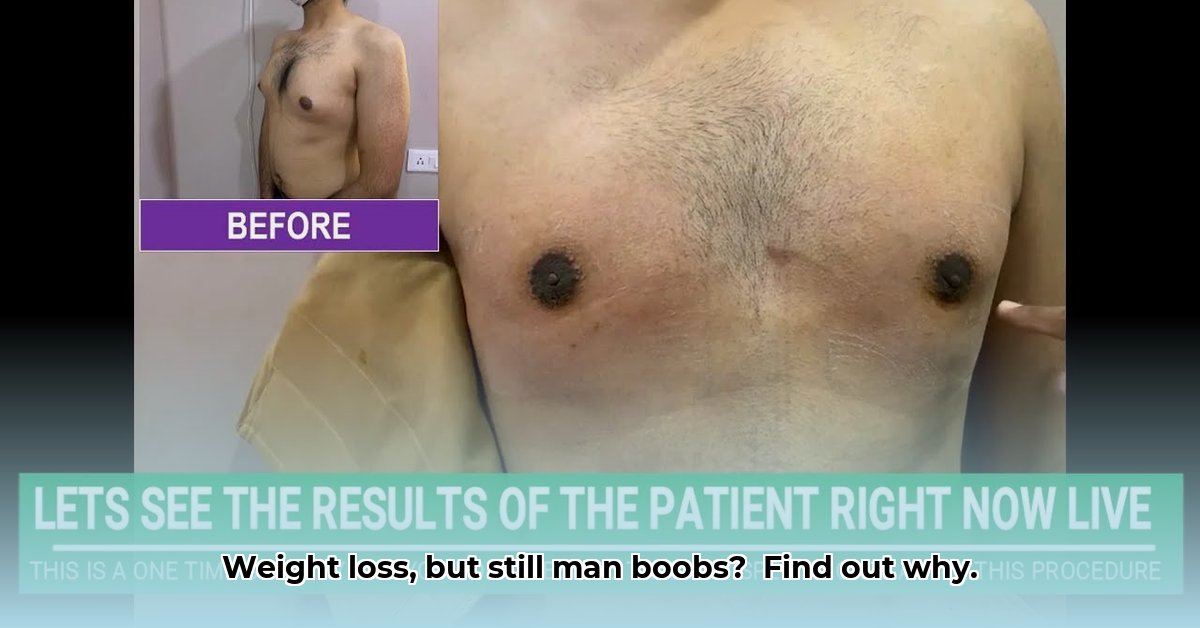
Understanding Gynecomastia and Why Weight Loss Isn't Always Enough
You’ve worked hard to lose weight, and you deserve to feel proud of your accomplishment. However, sometimes stubborn chest tissue remains, a condition known as gynecomastia. This can be incredibly frustrating, especially after dedicating yourself to a healthy lifestyle. It's important to understand that gynecomastia isn't simply excess fat; it's often caused by an imbalance of hormones, primarily estrogen and testosterone. While weight loss can reduce adipose tissue (fat), it won't address the underlying glandular tissue that contributes to gynecomastia.
Fat vs. Glandular Tissue: The Key Difference
Think of your breast tissue as having two layers: the outer layer, comprised of adipose tissue (fat), and an inner layer of glandular tissue. Weight loss primarily affects the outer layer. Gynecomastia, however, involves the inner glandular layer, often caused by hormonal fluctuations rather than excess weight. This distinction is crucial because effective treatment requires addressing the specific type of tissue causing the enlargement. This is why diet and exercise alone are often insufficient to resolve gynecomastia.
Treatment Options: Tailoring Your Approach
Fortunately, effective treatment options exist for gynecomastia. The best approach depends on the type and amount of tissue involved, as diagnosed by a healthcare professional.
Surgical Options
- Liposuction: This minimally invasive procedure uses suction to remove excess fat. It's best suited for cases primarily involving adipose tissue.
- Surgical Excision (Mastectomy for Gynecomastia): This more involved surgery directly removes excess glandular tissue. It's the preferred option for cases predominantly involving glandular tissue.
- Combination Approach: Many cases benefit from a combination of liposuction and excision, allowing for precise targeting of both fat and glandular tissue. A skilled surgeon will determine the optimal combination for your individual needs.
Choosing the Right Surgical Path: A Personalized Plan
Selecting the most appropriate procedure is a crucial step. A comprehensive consultation is essential. Your surgeon will conduct a thorough examination, often including imaging, to assess the composition of your breast tissue and determine the most effective treatment strategy. Open communication with your surgeon regarding your expectations and concerns is vital to ensure the best possible outcome.
The Emotional Impact: Addressing Your Concerns
Beyond the physical aspect, gynecomastia can significantly impact self-esteem and confidence. It's perfectly valid to feel frustrated or self-conscious. Don't hesitate to discuss your emotional well-being with your doctor or a therapist; they can provide support and guidance throughout your treatment journey. Remember, you are not alone in this, and help is available.
Recovery and Healing: What to Expect
Recovery time varies depending on the chosen procedure and individual healing response. Your surgeon will provide detailed post-operative instructions, including pain management, activity restrictions, and hygiene protocols. Patience and adherence to these instructions are vital for optimal results and minimizing complications.
When to Seek Medical Attention: Don't Delay
If you're concerned about breast enlargement, schedule a consultation with a physician or surgeon. Early diagnosis and intervention often lead to better outcomes. Don't let discomfort or self-consciousness prevent you from seeking the care you deserve.
Understanding the Risks: A Balanced Perspective
Like any surgical procedure, gynecomastia treatment carries potential risks, including infection, scarring, and nerve damage. However, these risks are generally low, and advancements in surgical techniques continually improve safety and efficacy. Your surgeon will clearly outline these risks during your consultation, allowing you to make an informed decision based on a complete understanding of the potential benefits and drawbacks.
How to Choose Between Liposuction and Excision for Gynecomastia
Key Considerations:
- Tissue Composition: The primary factor determining the best treatment approach is the proportion of fat versus glandular tissue.
- Severity of Gynecomastia: Mild cases may respond to liposuction, while more severe cases often benefit from excision or a combined approach.
- Individual Preferences: Your personal preferences, including risk tolerance and recovery expectations, should be considered in consultation with your surgeon.
Liposuction vs. Excision: A Detailed Comparison
This comparison highlights the key differences between liposuction and excision to help you and your surgeon determine the most suitable treatment option.
| Feature | Liposuction | Excision |
|---|---|---|
| Invasiveness | Minimally invasive | More invasive |
| Recovery Time | Shorter | Longer |
| Scarring | Minimal | More noticeable |
| Cost | Generally less expensive | Generally more expensive |
| Tissue Targeted | Adipose (fat) tissue | Glandular tissue |
| Effectiveness | Effective for pseudogynecomastia (fat-related) | Effective for true gynecomastia (glandular) |
Beyond Surgery: Exploring Non-Surgical Options
Before considering surgery, explore non-surgical options with your doctor. These may include treatments like CoolSculpting or Kybella, which can reduce localized fat deposits. However, it's important to remember that these techniques don't address glandular tissue.
Post-Operative Care: Optimizing Your Recovery
Regardless of the chosen procedure, diligent adherence to post-operative care instructions is crucial. This typically involves wearing compression garments, managing pain, restricting strenuous activity, and maintaining good hygiene. Your surgeon will provide comprehensive guidance to ensure a smooth recovery and the best possible outcome.